Yes, Humana Insurance does offer coverage for teen mental health treatment in California.
At Key Healthcare, we understand parents’ concerns when looking for mental health treatment for their teens in California.
If you have a Humana Insurance policy, you might wonder if it covers teen mental health treatment in California. This blog was created by our admission director, Sarah Carillo, to give a full overview of how Humana supports adolescent mental health care. It provides details on plan coverage, out-of-pocket costs, and the services that are covered. Our goal is to make this process simple and clear, allowing you to focus on getting your child the care they need.
What You Need to Know About California Humana Insurance?
As the third-largest healthcare company in the U.S., Humana serves over 13 million customers. It offers various plans like HMO, PPO, POS, and EPO, giving people flexibility in choosing doctors and coverage levels. These include Medicare Advantage, Medicaid, individual and family health plans, and supplemental insurance options. Since each plan may cover teen mental health treatment differently, understanding your specific policy is key.
After coverage is confirmed and authorization is received, we will work with you to schedule your teen’s treatment. This ensures they receive timely and effective care
Here is a list of Humana’s main plan types:
- Medicare Advantage Plans: Mainly cover mental health for people over 65 or those with certain disabilities.
- Medicaid Plans: Full coverage for low-income families and individuals.
- Individual and Family Plans: Health coverage for people under 65 who do not qualify for Medicare.
- Medigap (Medicare Supplement): Adds to Original Medicare by covering out-of-pocket costs for approved services.
- Supplemental Insurance: Provides extra coverage for dental, vision, and other special needs.
Does My Humana Insurance Cover Teen Mental Health Treatment in California?
Yes, Humana covers many treatments for teen mental health, but the specific coverage depends on your plan. To check your Humana insurance policy with us, simply fill out the verification form on our website, and we will handle the rest. We work directly with Humana to confirm all services are covered and to inform you of any out-of-pocket costs before treatment starts.
How to Fill Out the Insurance Verification Form for Teen Mental Health Treatment at Key Healthcare?

- Step 1: Enter your teen’s full name.
- Step 2: Add your email for updates.
- Step 3: Enter your phone number for follow-ups.
- Step 4: Add your teen’s date of birth.
- Step 5: Enter your name as the parent or guardian.
- Step 6: State if you are the main policyholder.
- Step 7: Name your insurance provider (e.g., Humana One).
- Step 8: Choose your plan type (HMO, PPO, etc.).
- Step 9: Upload images of the front and back of your insurance card.
- Step 10: State the type of treatment your teen needs (e.g., inpatient, outpatient).
- Step 11: Submit the form.

Once a parent submits the insurance verification form, our admissions team reviews the Humana plan. We check the coverage for mental health services, like inpatient, outpatient, and therapy options. We also confirm that your teen’s treatment is covered and determine any out-of-pocket costs, such as copays or deductibles.
If preapproval is needed, we submit all the required documents to Humana for you. This includes the treatment plan and details on medical need, which helps ensure a smooth and fast approval.
We will give you regular updates on your insurance approval status. If an issue like a denial occurs, we will help you with the appeal process and resubmit the needed information to get coverage.
What Services Does Humana Insurance Cover for Teen Mental Health Treatment in California?
Teen Inpatient and Outpatient Treatment
Humana Insurance provides full coverage for both inpatient and outpatient teen treatment. These services can include:
- Detoxification Services: Medical support and supervision during the withdrawal process.
- Live-in Rehab: Focused, planned care at an inpatient facility that may last from 30 to 90 days or more.
- Outpatient Programs: Flexible options for teens not needing 24/7 medical care. Humana covers Teen Intensive Outpatient Programs (IOP) and Adolescent Partial Hospitalization Programs (PHP). These programs give teens support while letting them return home at night.”
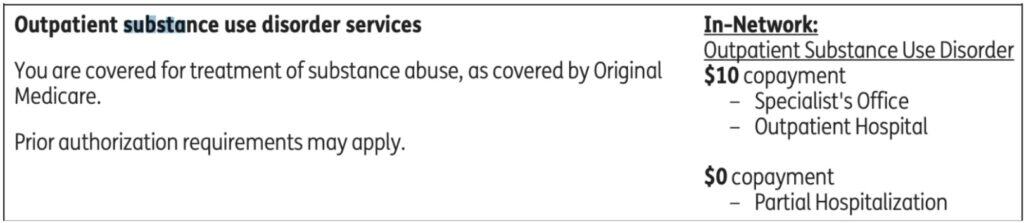
Outpatient services in California are covered by Humana plans. For in-network services, a $10 copayment applies to specialist visits, while day treatment has a $0 copayment.
Medication-Assisted Treatment (MAT)
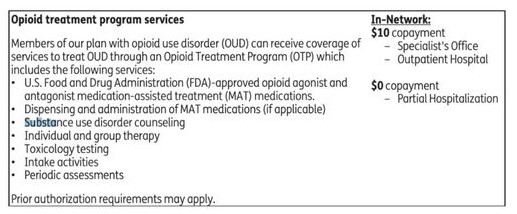
Humana coverage includes FDA-approved medications like methadone, buprenorphine, and naltrexone. A $10 copayment may apply for services at a specialist’s office under Humana’s plan, but day treatment services often have no extra cost.
Counseling and Therapy
Humana insurance plans cover individual, group, and family therapy for teens. These sessions are vital for addressing factors that contribute to teen mental health disorders. Therapy is offered in both inpatient and outpatient settings and is key for long-term support and recovery.
Beyond Humana, we also partner with other insurers, including Blue Cross Blue Shield of Arizona, Cigna , Aetna, Kaiser, GEHA, UMR, and Magellan.
Will My Humana Gold Plus H5619-021 (HMO) member Plan Cover Mental Health Issues?
Yes, most Humana plans, including Gold Plus, cover conditions that occur at the same time. This means treatment can be received if your teen has both mental health issues (like anxiety or depression) and other problems.
What are Medicare Part B Coverage for Teen Mental Health Services?
Medicare Part B (Medical Insurance) helps cover many teen mental health services that are typically received outside a hospital. These settings may include a clinic, doctor’s office, or hospital outpatient department. If your doctor accepts the assignment, Part B helps cover the following outpatient mental health services:
- A single “Welcome to Medicare” preventive visit in your first 12 months with Part B, which includes a depression risk assessment.
- Annual depression screening is provided once per year.
- Family counseling, if it is part of your teen’s treatment plan.”
- Teenage Psychiatric evaluations to assess mental health needs.
- Medication management for mental health conditions.
- Diagnostic tests related to mental health care.
- An annual “Wellness” visit, which allows you to discuss any mental health concerns or changes with your doctor.
Additionally, Part B may cover participation in a day treatment program if you meet certain criteria and a doctor confirms you would otherwise need inpatient treatment.
Note: If you have a Medicare Advantage (Part C) plan might offer extra mental health benefits not covered by Original Medicare, such as counseling. You should check the details of your plan for these extra benefits.
Do I Need Pre-Authorization for Teen Inpatient and Teen Outpatient?
For many mental health treatments, especially inpatient or live-in care, Humana may require pre-authorization. This preapproval process ensures that the treatment is medically necessary and follows the plan’s coverage guidelines.
At Key Healthcare, we know the insurance pre-authorization process can feel difficult, but it is a key step for ensuring your teen gets timely and full care. Humana requires preapproval for many behavioral health services, including inpatient and outpatient mental health treatments. Here is what you should know about the process and how we help you.
Step 1: Initiating Pre-Authorization
Pre-authorization, or preapproval, is needed to confirm that the requested treatment is medically necessary and covered by your Humana plan. At Key Healthcare, we manage this process for you. After a treatment plan is made for your teen, the preapproval request is submitted to Humana by us.
You can also start this process by logging into Humana’s member portal, where there is an option to request preapproval directly.
Step 2: Information Required for Pre-Authorization
Humana needs detailed information to approve a pre-authorization request. This includes:
- Member Details: Full name, date of birth, and Humana insurance ID number.
- Provider Details: The provider’s name, National Provider Identifier (NPI), and contact information.
- Service Details: Codes for diagnosis (ICD-10) and services (CPT/HCPCS) that describe the requested care (e.g., inpatient or outpatient rehab, detox, therapy).
- Medical Necessity: A statement from the healthcare provider explaining why the treatment is medically needed for the patient.
At Key Healthcare, we ensure all the necessary documents (e.g., medical records, progress notes, assessments, lab reports, etc.) and information are submitted, reducing the chance of delays or denials.
Step 3: Expected Response Time
After a pre-authorization request is submitted, Humana usually responds within 72 hours for standard requests. For urgent situations where a delay could risk your teen’s health, a faster review will be done within 24 hours. Our team at Key Healthcare ensures that any urgent requests are flagged and handled quickly.
Step 4: How We Submit Pre-Authorization
Pre-authorization requests are faxed to Humana’s Behavioral Health UM team at 469-913-6941. In urgent cases, we suggest calling Humana’s customer service line to make sure the request is processed right away. At Key Healthcare, we manage this entire process and keep in touch with Humana to update you on the approval status.
Step 5: What Happens If Pre-Authorization is Denied
If Humana denies a pre-authorization request, you have the right to appeal the decision. Our team will work with Humana to fix any issues by submitting more medical documents or requesting a review with their medical team. If needed, we will guide you through the appeals process to ensure that your teen gets the care they need.
At Key Healthcare, we handle the entire pre-authorization process for you. Our admissions team submits the needed documents to Humana for approval, including your teen’s diagnosis and proposed treatment plan. This reduces delays and helps your teen’s treatment begin as soon as possible.
If you need help with a claim or face a denial, our experienced staff will work directly with Humana to appeal the decision. This includes gathering any additional medical documents and, if necessary, asking for a peer-to-peer review with Humana’s medical team.
What Out-of-Pocket Costs Should I Expect from California Humana Insurance?

Your out-of-pocket costs will depend on your specific plan and may include:
- Co-payments: Fixed fees for services such as therapy.
- Deductibles: The amount you must pay before your insurance starts to cover services.
- Co-insurance: A percentage of costs that you share with the insurer after your deductible is met.
Here are the details about Medicare Part A and Part B costs, are listed below. This can give you an idea of possible out-of-pocket expenses for Humana plans, which often have similar structures. Here’s a summary of what it states:
Medicare Part A
- Premium: Most people who worked for at least 10 years and paid Social Security taxes do not pay a Part A premium.
- Deductible and Coinsurance:
- $1,632 deductible for each benefit period.
- Days 1–60: No coinsurance.
- Days 61–90: $408 coinsurance per day.
- Days 91 and beyond: $816 coinsurance per “lifetime reserve day” for up to 60 days.
After your lifetime reserve days are used, you must pay all costs.
Medicare Part B
- Premium: The standard premium is $174.70 per month in 2024, but it can be higher depending on your income.
- Deductible and Coinsurance:
- In 2024, the deductible is $240. After it is met, you’ll typically pay 20% coinsurance for most doctor services, outpatient therapy, and durable medical equipment (DME).”
Annual Maximum Out-of-Pocket Costs
- Original Medicare does not have a maximum out-of-pocket limit.
For Humana plans, such as Medicare Advantage, your out-of-pocket expenses are affected by the deductible and coinsurance. Whether there is an annual out-of-pocket maximum can vary by plan type.
What Adolescent Mental Health Services is Not Covered by Humana Insurance?
Some teen mental health services are not covered by Medicare, whether inpatient or outpatient. These include:
- Transportation to or from the Key Healthcare live-in treatment center
- A private room, unless it is considered medically necessary
- Private duty nursing services
- Extras like a phone or television in your room
- Personal items, such as toothpaste, socks, or razors
Key Healthcare Mental Health Treatment for Teens with Humana Coverage
Humana covers treatment for a wide range of mental health disorders, including:
- Teen Anxiety and Teen Depression
- Adolescent Bipolar Disorder
- Teen PTSD (Post-Traumatic Stress Disorder)
- Teen ADHD (Attention-Deficit/Hyperactivity Disorder)
- Teen Eating Disorders
- Oppositional Defiant Disorder (ODD)
- Teen Obsessive-Compulsive Disorder (OCD)
If your teen is struggling with anxiety, depression, ADHD, bipolar disorder, or other behavioral health issues, Humana’s benefits for behavioral health include:
- Psychiatric evaluations and diagnoses
- Individual and family counseling
- Teen Cognitive Behavioral Therapy (CBT)
- Medication management for mental health disorders
- Inpatient mental health services for teens who need intensive care and monitoring
Humana plans also cover telehealth services for mental health diagnoses, evaluations, and treatments. These remote options let teens receive care from home, which is often easier and more accessible for families.
Please contact us if you have more questions or need help checking your Humana coverage. We are here to support you every step of the way to ensure your teen receives the care they need.
Conclusion
At Key Healthcare, your teen’s health is our priority, and we work to make the financial side of treatment simple. With Humana’s full coverage and our dedicated support team, you can focus on your teen’s recovery journey. Contact us today to get started on verifying your coverage and enrolling your teen in the best treatment plan available.
Frequently Asked Questions
Relapse can be part of recovery, and Humana often covers additional treatment if your teen requires further care after a relapse.
Does Humana Cover In-Network and Out-of-Network Providers?
Humana PPO and POS plans usually cover out-of-network providers, though at a lower rate. HMO plans generally require you to stay in-network for coverage.
Can My Teen’s Mental Health Treatment Be Covered if They Are Out of State?
Humana may cover out-of-state treatment, depending on your specific plan and whether the facility is in-network.
Can I Expect Follow-Up Care to Be Covered?
Yes, many Humana plans cover aftercare services like follow-up therapy, outpatient counseling, and support groups to help maintain recovery after treatment is completed.